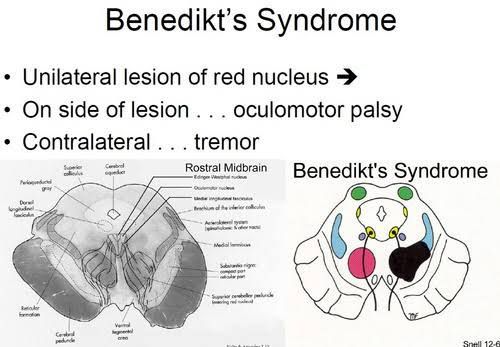
Benedikt Syndrome: A Classic Midbrain Stroke Syndrome
Benedikt syndrome is a rare posterior circulation stroke syndrome characterized by a distinctive combination of ipsilateral oculomotor (III) nerve palsy and contralateral movement disorders (tremor, ataxia), often with sensory loss. This reflects a focal lesion in the midbrain tegmentum, typically from occlusion of paramedian branches of the posterior cerebral or basilar arteries.
1. Historical Background and Eponym
Moritz Benedikt (1835–1920) was an Austro-Hungarian neurologist and one of the founders of criminal anthropology, hypothesizing a “moral center” in the occipital cortex .
He coined the term Darsonvalisation for high-frequency electrotherapy (1899) and even wrote on dowsing methods .
In 1889, Benedikt described the midbrain syndrome bearing his name, linking oculomotor fascicle involvement with red nucleus damage to explain the crossed signs .
2. Anatomy & Pathophysiology
A lesion in the paramedian midbrain tegmentum affects:
Oculomotor nerve fibers or nucleus → ipsilateral ptosis, “down and out” eye, pupillary involvement
Red nucleus and superior cerebellar peduncle → contralateral intention tremor, ataxia, dysmetria
Medial lemniscus (sometimes) → contralateral loss of proprioception & vibration
Etiologies include:
Ischemic infarct (PCA paramedian branches or basilar perforators)
Hemorrhage
Neoplasm
Infection (e.g., tuberculoma)
3. Clinical Features
Ipsilateral III-nerve palsy:
Ptosis
“Down and out” eye position
Mydriasis or miosis (pupillary involvement)
Loss of accommodation
Contralateral movement and cerebellar signs:
Intention tremor of hand/foot, often rhythmic, worsening with emotion or voluntary movement, absent during sleep
Dysmetria, ataxia
Contralateral sensory loss (if medial lemniscus involved):
Impaired vibration and joint position sense
4. Differential Diagnosis
5. Diagnosis
Clinical exam: crossed signs as above
MRI brainstem: focal lesion in paramedian tegmentum
Vascular imaging (MRA/CTA/angiography): PCA or basilar branch occlusion
6. Management & Prognosis
Acute stroke care: thrombolysis or thrombectomy when indicated; antiplatelet/anticoagulation and risk factor control
Supportive therapy:
Physical/occupational therapy for ataxia and tremor
Ophthalmologic interventions for persistent III-nerve palsy (e.g., ptosis crutch, prism lenses)
Pharmacologic tremor management: clonazepam, propranolol, levodopa in select cases
Prognosis varies with lesion size and cause; oculomotor deficits may partially recover, but tremor and ataxia often persist chronically.
7. Summary Table: Benedikt Syndrome Overview
8. Conclusion
Benedikt syndrome exemplifies the precision of crossed brainstem localization—oculomotor signs on one side, cerebellar/movement disturbances on the other. Moritz Benedikt’s 19th-century insights laid the foundation for modern understanding of midbrain stroke syndromes. Prompt recognition guides targeted imaging, acute stroke management, and tailored rehabilitation, improving functional outcomes in this uncommon but instructive neurological condition.
Comment