Horner’s Syndrome: Recognizing a Disruption in Sympathetic Supply
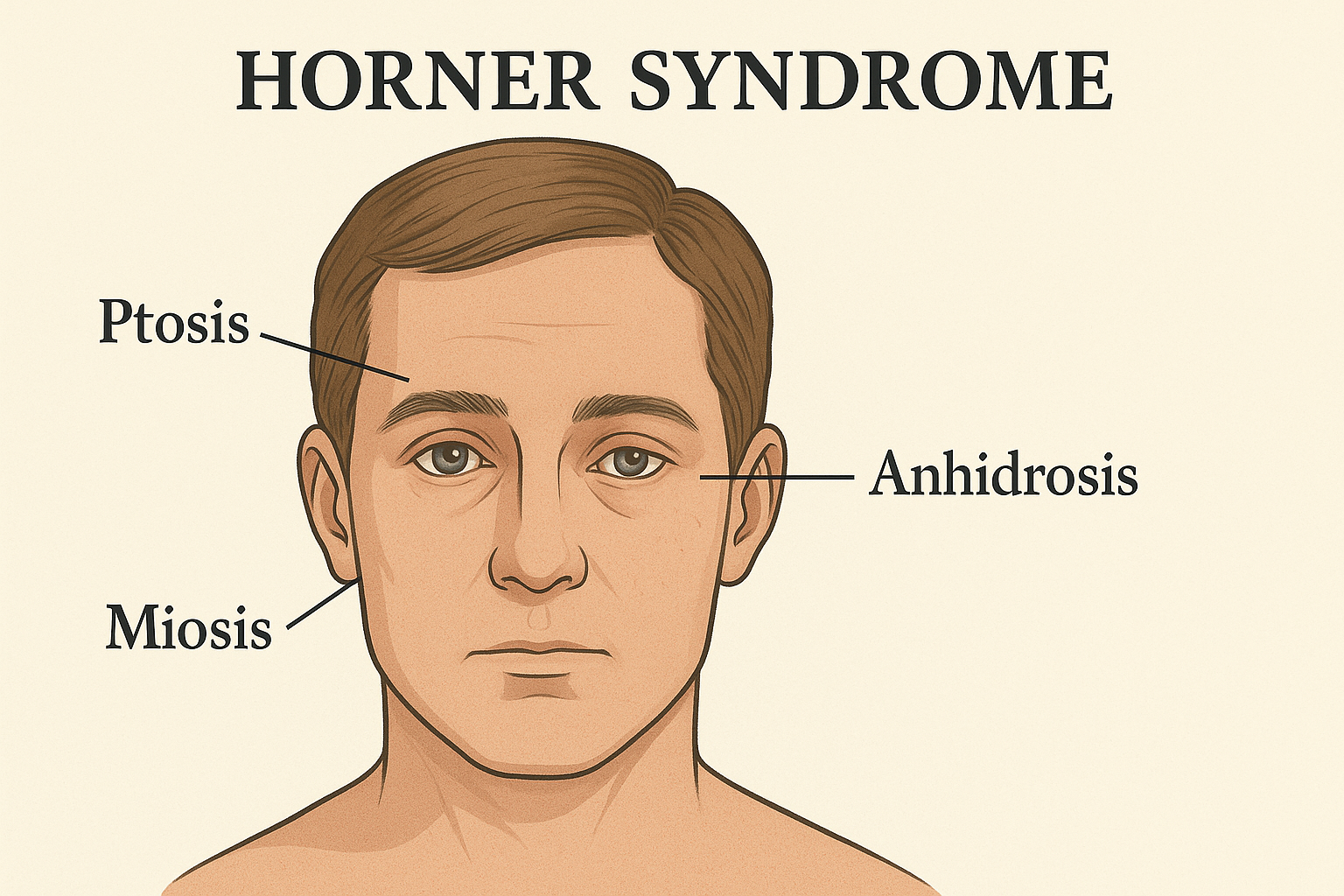
Horner’s syndrome arises from a lesion along the oculosympathetic pathway, leading to a distinctive triad of ptosis, miosis, and anhidrosis, often with subtle additional signs. Although sometimes benign, it can herald serious disease.
1. Historical Background and Eponym
First systematically described in 1869 by Swiss ophthalmologist Johann Friedrich Horner, its features were previously noted by Claude Bernard, François pourfour du Petit, and others. Horner’s definitive description—involving eyelid droop, pupil constriction, mild enophthalmos, and facial dryness—earned him lasting linkage with the condition.
2. Clinical Features
The hallmark triad includes:
Ptosis: Mild drooping of the upper eyelid due to Müller’s muscle paralysis
Miosis: Narrowing of the pupil, with normal light response but slow dilation in darkness
Anhidrosis: Reduced facial sweating on the affected side (variable depending on lesion site)
Additional signs may include:
Pseudo-enophthalmos: Eye appears sunken due to ptosis
Facial flushing or bloodshot eye due to loss of sympathetic vasoconstriction
Heterochromia iridis in congenital cases (lighter iris on the affected side)
3. Anatomy & Pathophysiology
The three-neuron pathway:
Central (first-order): Hypothalamus → C8–T2 spinal levels
Preganglionic (second-order): Spinal cord → superior cervical ganglion (via apex of lung)
Postganglionic (third-order): Superior cervical ganglion → cavernous sinus → eye
Lesion locations and features:
Central lesions (e.g., brainstem stroke, demyelination): Full-face anhidrosis + possible neurological signs
Preganglionic lesions (e.g., Pancoast tumor, thoracic surgery): Face/upper body sweating loss + arm symptoms
Postganglionic lesions (e.g., carotid dissection, cavernous sinus diseases): Little or no facial sweating change; isolated ptosis/miosis
4. Causes by Location
5. Diagnosis
Clinical assessment confirms the triad, with special attention to:
Anisocoria more pronounced in dim light (due to miosis)
Ptosis affecting Müller’s muscle (not levator; spares frontalis)
Ipsilateral anhidrosis (assessed by history/exam)
Pharmacological tests (where available) aid diagnosis:
Apraclonidine drops dilate the affected pupil
Cocaine drops fail to dilate the Horner pupil
Hydroxyamphetamine drops help localize lesion site (pre- or postganglionic)
Imaging guidance:
MRI/MRA of brainstem, neck, chest
Chest CT for suspected Pancoast tumors
Carotid imaging for dissection suspicion
6. Management
Focus is on finding and treating the underlying cause:
Vascular causes: Stroke or dissection protocols
Tumors: Referral to oncology or surgery
Immune or inflammatory: Appropriate medical therapy
No direct therapy exists for the syndrome itself. Eye care, ptosis support, or cosmetic measures may be considered.
7. Summary Table: Horner’s Syndrome at a Glance
8. Why It Matters
Horner syndrome is more than an ocular oddity—it often constitutes a red flag for serious vascular, neurological, or malignant diseases. Early recognition and localization can lead to life-saving diagnoses, such as carotid dissection or lung apex tumors.
Comment