Sheehan Syndrome: Postpartum Pituitary Necrosis and Lifelong Hypopituitarism
Sheehan Syndrome (SS) is a serious endocrine disorder caused by ischemic necrosis of the anterior pituitary following severe postpartum hemorrhage. It results in varying degrees of hypopituitarism, which may present acutely or develop insidiously years after delivery. First clearly delineated by British pathologist Harold Leeming Sheehan, its history actually traces back to earlier observations by Glinski and Simmonds.
1. Historical Background and Eponym
1913: Polish pathologist Leon Konrad Glinski reported two postpartum women with extensive pituitary necrosis post-mortem, attributing it to hypophyseal artery thrombosis .
1914: German pathologist Morris Simmonds described chronic hypopituitarism after puerperal sepsis, noting progressive pituitary atrophy—later called Simmonds disease .
1937: Sheehan, as pathologist at Glasgow Royal Maternity Hospital, studied 76 postpartum autopsies and found that 12 cases of hemorrhagic shock (not sepsis) were linked to anterior pituitary necrosis. This work established the obstetric ischemia hypothesis.
1949: Sheehan and Summers clarified that emaciation and prematurity of senescence were not essential features, helping standardize the eponym “Sheehan syndrome” .
2. Pathophysiology
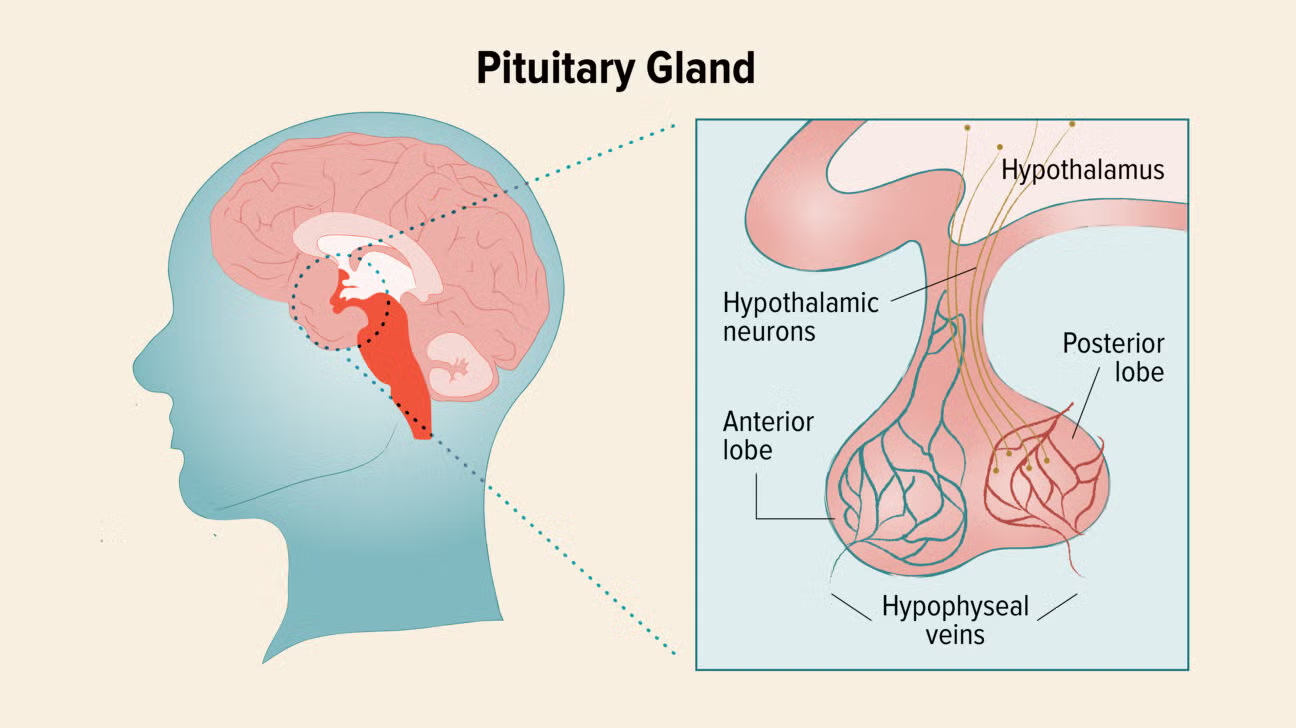
During pregnancy, the anterior pituitary enlarges up to twice its normal size due to lactotroph hyperplasia.
Postpartum shock and hemorrhage trigger ischemia via portal vessel thrombosis and vasospasm, leading to necrosis and loss of hormone-producing cells .
The posterior pituitary is typically spared due to its direct arterial blood supply.
If damage is severe, central diabetes insipidus (ADH deficiency) may develop, though it is rare .
3. Clinical Features
Early/Postpartum Findings
Failure to lactate (agalactorrhea)
Amenorrhea (absent menses)
Breast involution, fatigue, persistent hypotension
Late or Chronic Symptoms
Secondary adrenal insufficiency (low ACTH): fatigue, hyponatremia, risk of adrenal crisis
Hypothyroidism (low TSH): cold intolerance, lethargy
Gonadotropin deficiency: amenorrhea, infertility, loss of libido
Growth hormone deficiency: reduced muscle mass, low energy
Anemia, haematological abnormalities
4. Diagnosis
Clinical suspicion after severe postpartum hemorrhage, especially when lactation and menstruation fail to resume.
Hormonal assays: low ACTH, TSH, LH, FSH, growth hormone, and prolactin.
MRI findings: in acute cases, an enlarged/necrotic pituitary; chronic cases show “empty sella” or pituitary atrophy .
5. Differential Diagnosis
Lymphocytic hypophysitis
Pituitary adenomas or radiation-induced hypopituitarism
Simmonds disease from non-obstetric causes
6. Management and Prognosis
Lifelong hormone replacement:
Glucocorticoids (e.g., hydrocortisone) for adrenal insufficiency
Levothyroxine for hypothyroidism
Sex hormone replacement (estrogen/progesterone or testosterone)
Growth hormone in selected cases
Patients need endocrinologist-guided dose adjustments, especially during stress or illness.
Prognosis: Excellent if recognized early and treated; untreated adrenal insufficiency may be life-threatening.
7. Epidemiology and Public Health Impact
SS is now rare in high-resource settings but persists in low-resource areas where PPH remains a major cause of maternal mortality .
A UK study found SS represented 1.4% of hypopituitarism cases, while WHO estimated approximately 3 million affected women globally .
8. Summary Table: Sheehan Syndrome Snapshot
9. Conclusion
Sheehan Syndrome underscores the vital link between obstetric care and long-term endocrine health. It demonstrates how postpartum hemorrhage can silently compromise pituitary function, manifesting years after delivery.
Despite improved care, SS remains a neglected condition in resource-limited settings. Early recognition—particularly in women with lactation failure and amenorrhea after childbirth—combined with appropriate hormonal therapy can drastically improve outcomes. It stands as a powerful testament to the synergy of pathology, clinical vigilance, and endocrine medicine.
Comment